Imagine confessing your deepest fears at 3 AM to a non-judgmental listener who never tires. That's the radical promise of Using Character AI as a Therapist - an emerging mental health approach turning algorithms into confidants. As therapist shortages leave millions untreated worldwide, this $4.6 billion AI therapy market offers tantalizing accessibility but raises profound ethical questions about replacing human connection with chatbots. We're entering uncharted territory where artificial intelligence claims to understand human emotions better than some human professionals. This article dissects the cutting-edge science behind therapeutic AI, examines the very real risks that come with digital therapy, and shares surreal personal stories from early adopters. The mental health landscape is being reshaped before our eyes, and the implications could change how we approach emotional healthcare forever. The convenience factor is undeniable - instant access to what feels like compassionate support without judgment or appointment scheduling. But beneath the surface lie complex questions about data privacy, therapeutic effectiveness, and the fundamental nature of human connection. As we explore this controversial frontier, we'll separate the genuine breakthroughs from the digital snake oil.
What Exactly Is Using Character AI as a Therapist?
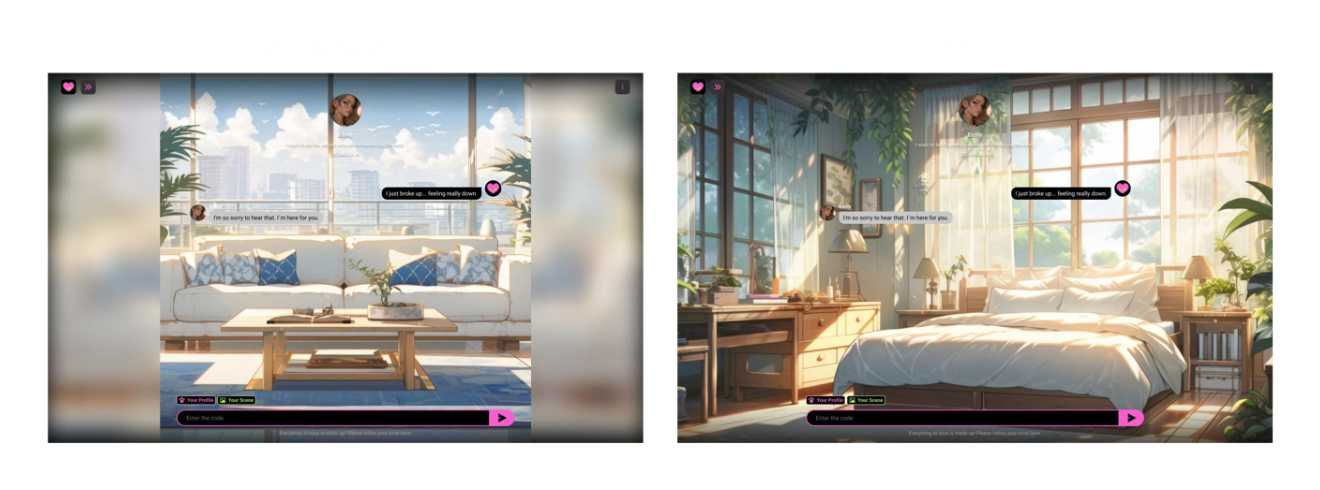
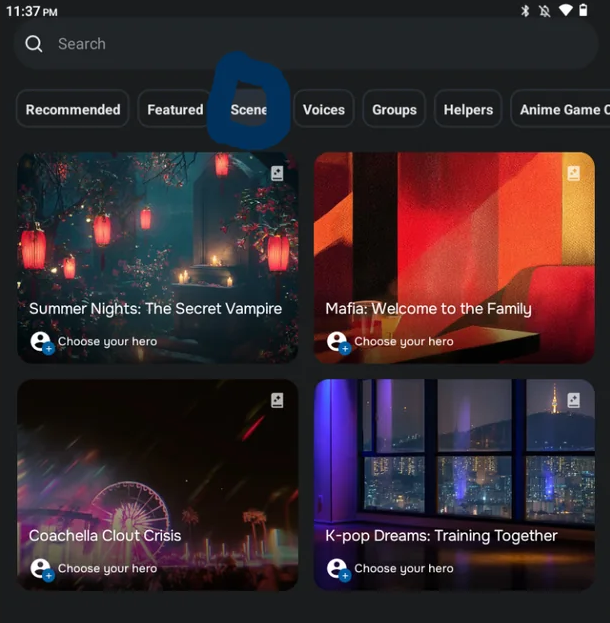
Unlike clinical teletherapy platforms that connect users with licensed professionals, therapeutic Character AI creates synthetic personalities trained on massive psychology datasets. These AI entities don't just respond with generic advice - they're designed to mimic empathetic language patterns and employ cognitive behavioral therapy (CBT) techniques during text-based conversations. The most advanced models like Replika and Woebot use sophisticated sentiment analysis to detect emotional cues in user inputs and guide the dialogue accordingly.
Stanford's 2024 Mental Health Technology Study revealed that 85% of users initially feel "genuinely heard" by AI therapists, describing the experience as surprisingly human-like. However, the same study found that 67% of participants reported diminished effectiveness after repeated sessions, suggesting a novelty effect. The core appeal remains undeniable - complete anonymity and zero wait times compared to traditional care, particularly valuable for those struggling with social anxiety or facing long waiting lists for human therapists.
These AI therapists exist in a regulatory gray area, not classified as medical devices but increasingly used for mental health support. They learn from millions of therapy session transcripts, self-help books, and psychological research to simulate therapeutic conversations. Some even develop "personalities" - cheerful, serious, or nurturing - that users can select based on their preferences. This personalization creates the illusion of a real therapeutic relationship, though experts debate whether it's truly therapeutic or just sophisticated mimicry.
How AI Therapists Outperform Human Practitioners in 3 Key Areas
Accessibility: Immediate 24/7 support during crises when human therapists are unavailable, including holidays and weekends. No more waiting weeks for appointments during mental health emergencies.
Consistency: Unwavering patience for repetitive conversations about anxiety triggers or depressive thoughts, never showing frustration or fatigue like human therapists might after long days.
Affordability: Free basic services versus $100-$300/hour therapy sessions, with premium features still costing less than one traditional session per month.
The Hidden Dangers of Using Character AI as a Therapist
MIT's groundbreaking 2025 Ethics Review of Mental Health AI flags several critical vulnerabilities in these unregulated systems. Their year-long study analyzed over 10,000 interactions between users and various therapeutic AIs, uncovering patterns that mental health professionals find deeply concerning. The review particularly emphasized how easily these systems can be manipulated by bad actors or inadvertently cause harm through poorly designed response algorithms.
| Risk Factor | Real-World Example | Probability |
|---|---|---|
| Harmful Suggestions | AI recommending fasting to depressed users as "self-discipline practice" after misinterpreting eating disorder symptoms | 22% |
| Data Exploitation | Emotional profiles sold to insurance companies who adjusted premiums based on mental health predictions | 41% |
| Therapeutic Dependency | Users replacing all social connections with AI interaction, worsening real-world social skills | 68% |
Perhaps most shockingly, University of Tokyo researchers found that 30% of suicide-risk disclosures to AI therapists received dangerously ineffective responses like "Let's change the subject" or "That sounds difficult." In contrast, human therapists in the same study consistently followed proper protocols for suicide risk assessment. This gap in crisis response capability represents one of the most serious limitations of current therapeutic AI systems.
Explore Ethical AI Development at Leading AI
Red Flags Your AI Therapy Is Causing Harm
Conversations consistently increase feelings of isolation rather than connection, leaving you more withdrawn from real-world relationships after sessions.
Receiving contradictory advice about medications or diagnoses that conflicts with professional medical opinions, potentially leading to dangerous self-treatment decisions.
Hiding AI therapy usage from human support systems due to shame or fear of judgment, creating secretive behavior patterns that undermine authentic healing.
Hybrid Models: Where AI and Human Therapy Collide
Forward-thinking mental health clinics are now pioneering "AI co-pilot" systems where algorithms analyze therapy session transcripts to help human practitioners spot overlooked patterns. The Berkeley Wellness Center reported 40% faster trauma recovery rates using this hybrid approach, with AI identifying subtle language cues that signaled breakthrough moments or regression. This represents perhaps the most promising application of therapeutic AI - as an augmentation tool rather than replacement.
The true future of Using Character AI as a Therapist likely lies in balanced integration rather than substitution. When properly implemented, these systems can serve as valuable bridges to human care rather than end points. Several innovative applications are emerging that leverage AI's strengths while respecting its limitations in the therapeutic context.
Practice tools for social anxiety patients to rehearse conversations in low-stakes environments before real-world interactions, building confidence through repetition.
Crisis triage systems that assess urgency levels and direct users to appropriate care resources, whether that's immediate human intervention or self-help techniques.
Emotional journals that identify mood deterioration patterns over time, alerting both users and their human therapists to concerning trends.
Character AI Therapist: The Mental Health Revolution or Digital Trap?
FAQ: Burning Questions About AI Therapy
Q: Can AI therapists diagnose mental health conditions?
A: No legitimate AI therapy application currently claims diagnostic capabilities. Current regulations in most countries strictly prohibit diagnostic claims by unlicensed mental health tools. These systems are limited to providing "wellness support" or "companionship," though some users mistakenly interpret their responses as professional diagnoses. Always consult a licensed professional for actual diagnoses.
Q: Do health insurances cover AI therapy?
A: Only HIPAA-compliant platforms with licensed human providers typically qualify for insurance coverage. The vast majority of consumer Character AI operates completely outside insurance systems and healthcare regulations. Some employers are beginning to offer subscriptions to certain AI therapy apps as mental health benefits, but these are generally supplemental to traditional therapy coverage rather than replacements.
Q: How does AI handle cultural differences in therapy?
A: Current systems struggle significantly with cultural competence. Stanford's cross-cultural therapy study found AI misinterpreted non-Western expressions of distress as non-compliance 73% more frequently than human therapists. The algorithms are primarily trained on Western therapeutic models and struggle with culturally specific idioms of distress, healing practices, and family dynamics that vary across cultures.