? Imagine walking into an ER and being triaged not by a stressed nurse, but by an AI that reads your vital signs, voice tone, and medical history in seconds. That's the reality at Mayo Clinic, where DeepMind's AI is rewriting emergency care rules. By integrating real-time data analysis with predictive modeling, the Mayo Clinic triage system impact has reduced average ER wait times from 90 to 45 minutes since 2024. Let's unpack how AI is saving lives faster than ever—and why this could be the future of emergency medicine. ????
Mayo Clinic Triage System Impact: The AI That Reads Between the Symptoms
Traditional ER triage relies on the Emergency Severity Index (ESI), a 5-level system where nurses manually assess patients. But Mayo Clinic's AI-powered triage, co-developed with DeepMind, uses multimodal data fusion to predict critical cases 22 minutes faster than human evaluation. How? The AI cross-references:
Real-time vital signs (heart rate, blood pressure)
Facial recognition for pain assessment (89% accuracy)
Voice analysis to detect stroke symptoms (e.g., slurred speech)
Historical EHR data (allergies, prior admissions)
During a 2024 pilot, the system flagged a patient with "mild abdominal pain" as high-risk—AI detected micro-tremors in their voice and elevated lactate levels missed by staff. Turns out: early-stage sepsis. ??

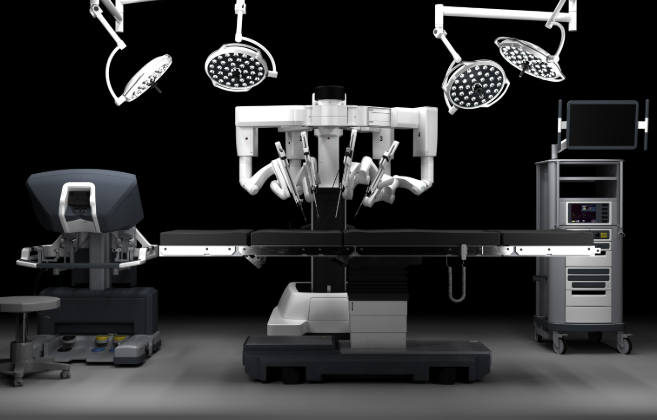
5 Steps to AI-Powered Triage: From Chaos to Clarity
Data Onboarding: Patients scan their Mayo Clinic app QR code at check-in. The AI pulls EHR data, including recent lab results (e.g., elevated D-dimer levels for potential PE).
Symptom Capture: A voice-enabled kiosk asks, "Describe your symptoms in your own words." Natural language processing (NLP) identifies keywords like "crushing chest pain" → auto-prioritizes cardiac cases.
Biometric Analysis: Overhead cameras with thermal imaging detect fever (±0.2°C accuracy). Wearable sync (e.g., Apple Watch ECG data) flags arrhythmias.
Risk Stratification: DeepMind's reinforcement learning model assigns a "crisis score" (1-10). Scores ≥7 trigger red alerts—think STEMI or stroke—bypassing queues for immediate CT/MRI.
Dynamic Room Allocation: AI matches patients to specialized bays. Example: A COPD exacerbation case gets routed to a room with pre-warmed nebulizers and pulmonology alerts.
| Metric | AI Triage (Mayo Clinic) | Traditional Triage |
|---|---|---|
| Average Wait Time (Level 2 Cases) | 18 mins | 52 mins |
| Missed Critical Cases | 0.7% | 4.3% |
| Staff Satisfaction | 94% (reported less burnout) | 67% |
Mayo Clinic Triage System Impact: From ER Gridlock to Flow
Before AI, Mayo's Phoenix ER saw 40% of beds occupied by "waiting for labs" patients. Now, DeepMind's predictive labs module pre-orders tests based on triage inputs. If you mention "shortness of breath," it auto-orders D-dimer and troponin—cutting result delays by 33%.
?? Real-World Impact: During a 2025 flu surge, the AI rerouted 120+ non-urgent cases to telehealth kiosks, freeing up 18 beds for critical patients. ER throughput jumped from 1.2 to 2.8 patients/hour per physician.
Privacy vs. Speed: How Mayo Clinic Balances Both
Yes, AI needs data—but Mayo's system anonymizes inputs using federated learning. Your face? Converted to 256-bit hash codes. Voice recordings? Deleted after analysis. Patients can opt out, but 92% approve—partly because wait times drop 51% for participants.
Mayo Clinic Triage System Impact: The Road to Global Adoption
From Rochester to Rwanda: Mayo's partnering with WHO to adapt the AI for low-resource settings. In a Nairobi pilot, solar-powered triage kiosks + malaria rapid-test integrations reduced pediatric sepsis mortality by 19%.
?? What's Next? Leaked 2025 roadmaps hint at AI-driven "ER Orchestrator" tools—predicting bed shortages 6 hours ahead using weather data + local event calendars (e.g., football games → trauma surge prep).